 In July, we published an article on the efficacy of cloth masks. Most of the testing research we cited required expensive industrial-quality equipment that makes it difficult for others who may not have the budgets to conduct their own tests. That’s why we were very interested in hearing about Duke University’s project to develop a low-cost measurement process for facemask efficacy in filtering expelled droplets during speech. This research was presented in a recent AATCC webinar by Dr. David Grass, Research Associate, Warren Group, Dept of Chemistry, Duke University, who views it as just the beginning of research into the topic.
In July, we published an article on the efficacy of cloth masks. Most of the testing research we cited required expensive industrial-quality equipment that makes it difficult for others who may not have the budgets to conduct their own tests. That’s why we were very interested in hearing about Duke University’s project to develop a low-cost measurement process for facemask efficacy in filtering expelled droplets during speech. This research was presented in a recent AATCC webinar by Dr. David Grass, Research Associate, Warren Group, Dept of Chemistry, Duke University, who views it as just the beginning of research into the topic.
This was the fourth in a series of PPE-related webinars conducted by AATCC. The first was recorded in late May and documented impact penetration testing that measures the amount of liquid that passes through a fabric under specified conditions for PPE and other water-resistant applications. The second, recorded in early June, documented standards for hydrostatic pressure testing for textiles, which is required for Level 2 and 3 medical gowns and drapes. And the third session, recorded in July, provided an overview of surgical masks and respirator industry standards, methods, and regulations. All are must-view sessions for health care professionals and anyone producing or interested in producing PPE.
That bring us to last week’s session, “Low-Cost Measurement of Facemask Efficacy for Filtering Expelled Droplets During Speech,” presented by Dr. Grass. We felt this was an especially important session since the Duke team was able to put together a system to test aspects of the efficacy of face masks that costs approximately $200 assuming the availability of a smartphone camera (in their case, a Samsung Galaxy S9). They also recommend purchasing high-quality safety glasses estimated at $150. This puts the system within reach of even the smallest of research department budgets. As you will see, the study documents the efficacy of different facemasks in filtering expelled droplets during speech, but also recommends other testing that could—and probably should—be done to take this research to the next level.
Dr. Grass started his presentation by noting that there was an unexpected amount of media coverage of the study but that too much of it was reported inaccurately, even by respected news outlets. To be sure we got it right, we gave Dr. Grass the opportunity to review it prior to publication! The full study can be found here.
It should be noted that testing was not COVID-19 specific, but rather to demonstrate why masks work as a physical barrier: what they protect against and how well depends on how much gets through them. Dr. Grass stated that, to his knowledge, this was the first testing of human activity and masks combined. Previous research used a variety of systems to expel air thorough the mask material and measure particles that passed through, as we outlined in our previous article.
System Components
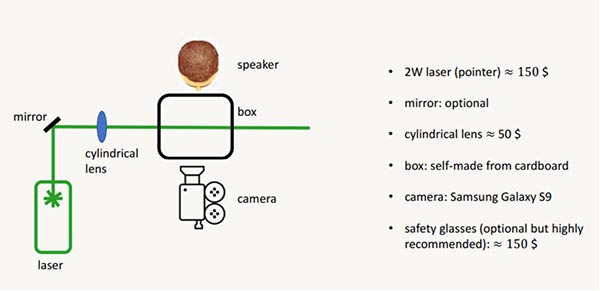
First, let’s take a look at the system components. Aside from high-quality safety glasses to protect participants’ eyes and the smartphone camera, the most expensive component is the laser. For purposes of this experiment, the team used a research grade 2W laser costing $150, but we believe that the same results can be achieved with a 2W laser that can be acquired on Amazon or eBay. Dr. Grass notes that a research-quality laser, like those used in other tests, are much more expensive.
The system has an optional mirror and a box made from cardboard, as well as a $50 cylindrical lens. The diagram below shows the setup:
Source: Dr. David Grass
Here’s another view:
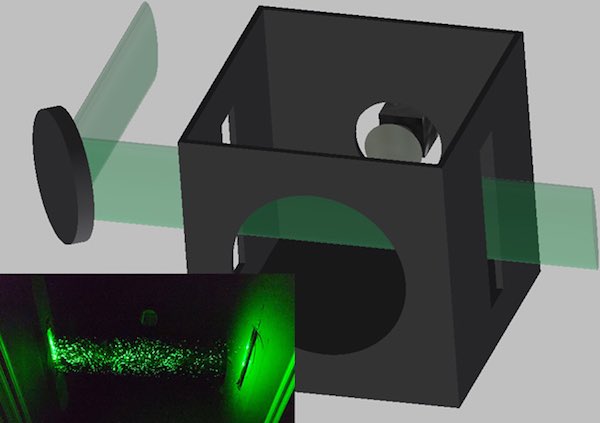
Source: https://advances.sciencemag.org/content/6/36/eabd3083/tab-figures-data
If the mirror is not used, the laser can be directly aligned with the smartphone camera.
Testing Process
Dr. Grass pointed out that no AATCC test methods were taken into consideration. They simply fitted different types of masks on a person’s face rather than placing material on a piece of testing equipment. Fourteen different mask types were tested as shown below:

Source: https://advances.sciencemag.org/content/6/36/eabd3083/tab-figures-data
These masks were acquired through the normal means a consumer might acquire them. One speaker repeated the sentence, “Stay healthy people,” three times as demonstrated in this YouTube video. Mask types 4, 12, and 13 were tested with four different speakers.
As the expelled droplets passed through the laser light source, and resulting photons were viewed and recorded by the smartphone camera, allowing analysis of the number of particles expelled, either without a mask or through various types of masks. Dr. Grass indicated that a conservative determination of the smallest droplet size that can been seen is 0.5 micrometers.
As we pointed out in our earlier article, “The [COVID-19] virus is primarily transmitted through what scientists call Flugge droplets, the droplets produced by humans coughing or sneezing—or even talking, singing, or other activities where breath is expelled. These droplets measure 0.5 to 10 microns. For reference purposes, a human hair ranges from 80 to 100 microns, so these droplets are tiny. But not as tiny as a virus particle, which also spreads the disease primarily by becoming airborne and inhaled. These particles are spheres with diameters of approximately 0.125 micron. Tiny, tiny, tiny!”
So the test system won’t be able to capture airborne virus particles, but still is quite useful in terms of droplets that most masks are thought to filter out. Also noted was that the system measures outbound droplets, not inbound. So the results indicate how you are protecting others more than it indicates how much the mask is protecting the wearer. This is also preliminary research on the topic and not meant to act as a recommendation, but rather as a basis for further research.
For example, as one questioner in the webinar pointed out, documenting the weave type and thread count for a cloth mask would also be useful, in addition to the fiber type.
Results
The actual published study has lots of technical detail on the results and the impact of the test configuration, which we won’t go into detail here. For example, Dr. Grass points out that the amount of droplets expelled that can actually be measured is gated by size, of course, and by the viewing area of the camera lens. A more expensive camera or wider angle lens could capture more droplets.
The chart below shows results by mask type:
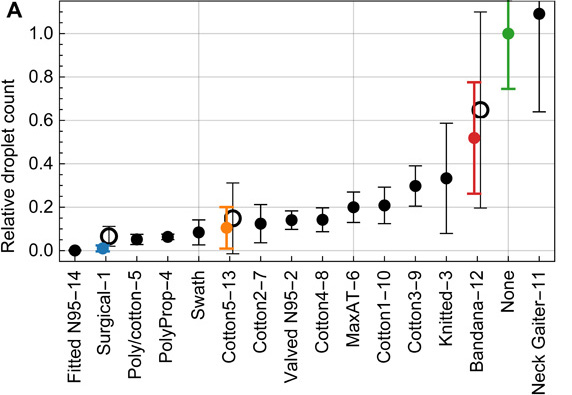
Source: https://advances.sciencemag.org/content/6/36/eabd3083/tab-figures-data
Each solid data point represents the mean and standard deviation (SD) over 10 trials for the same mask, normalized to the control trial (no mask), and tested by one speaker. Hollow data points are the mean and SDs of the relative counts over four speakers.
Best performing, of course, were fitted N95 masks and three-layer surgical masks. One alternative I have been using, because I like my knitted mask, is to insert a three-layer surgical mask in the filter pocket of the mask. That allows a more stylish mask with likely at least as much efficacy as a surgical mask.
Future Studies
Dr. Grass pointed out that future studies could look at droplets expelled when singing, coughing, sneezing, etc., to determine what the differences might be. And as we mentioned, more data could also be collected about the actual weave and thread count of the various masks, as well as fiber content. And data could be recorded about the age, gender, ethnicity, etc., of the speakers (or sneezers, etc.).
Since it looks like face coverings are likely to be with us for some time, all of this research is valuable in helping to guide health professionals, mask manufacturers and consumers about the efficacy of various mask types, and we commend Dr. Grass and the Duke team for their important efforts.











Discussion
Join the discussion Sign In or Become a Member, doing so is simple and free